Fibromialgia: Cosa devi sapere su cause, sintomi e trattamenti più efficaci!
La fibromialgia è una condizione complessa e spesso fraintesa, ha attraversato vari cambiamenti nella sua definizione e percezione nel corso degli anni. In questo approfondimento, scoprirai tutto ciò che la scienza e la medicina moderna sanno oggi.
Evoluzione e Storia della Fibromialgia
La fibromialgia fu inizialmente definita nel 1869 da Beard, il famoso psicologo che per primo definì la sindrome, come “esaurimento nervoso”. Passando attraverso le definizioni come “Panalgesia” nel 1978 e considerata un disturbo della soglia del dolore o “disnocipatia” negli anni successivi, la scoperta della vera natura della fibromialgia rimaneva comunque oscura. Nel 2008, un incontro di esperti italiani ha invece contribuito a delineare una definizione più approfondita: "Sindrome da Sensitizzazione Centrale". In termini più semplici, è emerso che il dolore cronico diffuso, la caratteristica predominante della fibromialgia, è il risultato dell'attivazione dei centri del dolore situati proprio all'interno del sistema nervoso. È da qui che deriva l'aggettivo "centrale".
Oggi la fibromialgia è considerata in tutto e per tutto una condizione di dolore cronico e sta acquisendo rilevanza anche tra i clinici più scettici
Fibromialgia in Numeri: Chi è più Colpito?
Le donne rappresentano il 90% dei casi di fibromialgia. A livello globale, circa il 2,7% della popolazione ne è affetto, con un picco tra i 40 e 60 anni. In Italia, l’incidenza sulla popolazione raggiunge il 5,5%.
Sintomi della Fibromialgia: Come si Manifesta?
Dal dolore diffuso alla stanchezza, dai disturbi del sonno alla cosiddetta “fibrofog”. Esiste un ampio spettro di sintomi associati alla fibromialgia che influenzano notevolmente la vita quotidiana. Vediamo quali sono i principali:
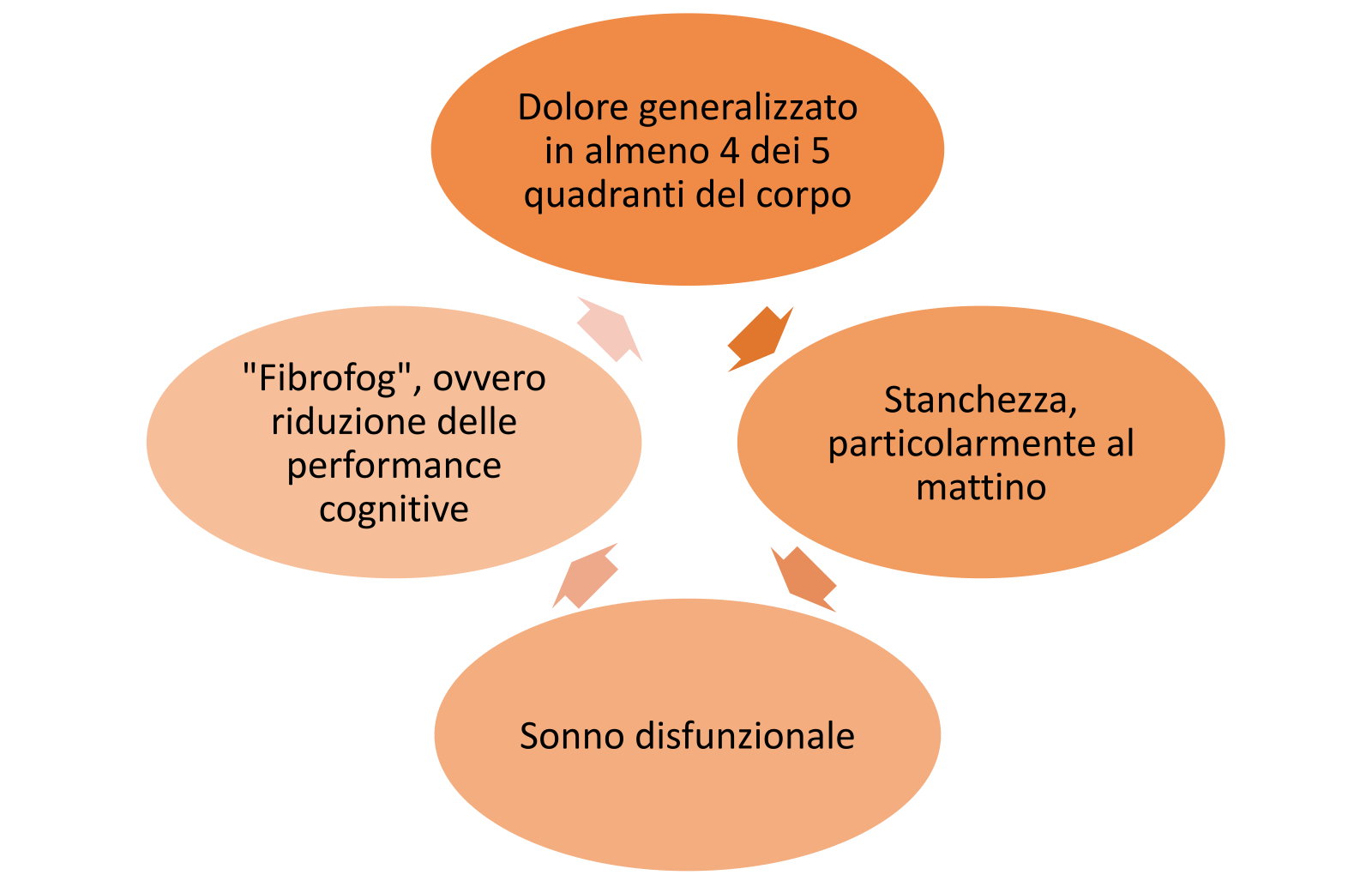
Dolore diffuso: Chi soffre di fibromialgia spesso avverte un dolore costante e pervasivo, che colpisce braccia, gambe e tronco. Questo dolore, che può variare in intensità, influisce sulla capacità di svolgere attività quotidiane come camminare, sollevare oggetti o persino alzarsi dal letto. Peggiora nei periodi di cambio stagione o nei periodi di maggiore stress.
Stanchezza estrema: La sensazione di fatica, specialmente al mattino, è così intensa che può rendere difficile iniziare la giornata, nonostante si possa aver dormito per molte ore.
Problemi di sonno: Anche se si dorme, il riposo potrebbe non essere profondo o ristoratore. Ciò comporta un senso di stanchezza e affaticamento cronico.
“Fibrofog”: Il cervello sembra funzionare a un ritmo più lento. Dimenticanze, difficoltà a concentrarsi e una sensazione di "nebbia mentale" sono comuni.
Oltre a questi sintomi principali, possono esserne presenti altri come: Problemi digestivi, Ansia, Bruciore intimo, Sensibilità agli odori, Secchezza e dolore agli occhi, ecc…
L'insieme di questi sintomi può avere un notevole impatto sulla vita quotidiana e lavorativa , compromettendo la capacità di svolgere compiti semplici, mantenere relazioni sociali e raggiungere obiettivi professionali. Pertanto, chi soffre di fibromialgia non ` solo alle prese con un disagio fisico, ma vive anche le sfide di un impatto emotivo e psicologico profondo.
Comprendere le Cause della Fibromialgia
So che il termine "fibromialgia" può suonare complesso e forse un po' intimidatorio. Ma voglio aiutarti a comprenderne le cause, che, in realtà, gli stessi medici stanno ancora cercando di delineare completamente. La fibromialgia è una condizione che ha molte possibili origini. Immaginate di cercare di risolvere un puzzle, ma non avete l'immagine di riferimento sulla scatola. Gli esperti stanno cercando di mettere insieme i pezzi, e alcune delle ipotesi principali formulate ad oggi includono:
Neurotrasmettitori Fuori Sincrono: I neurotrasmettitori sono sostanze chimiche nel nostro corpo che aiutano a inviare messaggi tra le cellule nervose. Si ritiene che nella fibromialgia ci possa essere un malfunzionamento in come questi messaggi vengono trasmessi
Un Sistema Nervoso "Troppo Sensibile": L'idea qui è che il sistema nervoso delle persone con fibromialgia potrebbe reagire in modo eccessivo ai segnali di dolore, rendendoli molto più intensi di quanto dovrebbero essere.

Problemi con l'Ipotalamo e l'Ipofisi: Queste sono due piccole parti del cervello che regolano molte funzioni nel nostro corpo, come la temperatura, la fame e lo stress. Cambiamenti in queste aree possono influenzare come percepiamo il dolore.
Genetica: Alcuni ricercatori pensano che ci possa essere un collegamento genetico nella fibromialgia. In particolare, alcune persone potrebbero avere geni che rendono il loro corpo più sensibile al dolore a causa di come il corpo usa la serotonina e la dopamina, due sostanze chimiche legate alla sensazione di dolore.
Infiammazione cronica a bassa intensità: Quando si parla di fibromialgia, l'infiammazione cronica sotto soglia gioca un ruolo fondamentale. Questo tipo di infiammazione, pur essendo più sottile e meno evidente rispetto a quella acuta, può contribuire alla genesi e al mantenimento del dolore cronico diffuso tipico della fibromialgia.
Il Microbiota Intestinale: Negli ultimi anni, alcune ricerche hanno evidenziato un legame tra il microbiota intestinale e diverse malattie, compresa la fibromialgia. Alterazioni nella composizione del microbiota possono influenzare il sistema immunitario, contribuendo all'infiammazione cronica e potenzialmente acutizzando i sintomi della fibromialgia.
La Matrice Extracellulare: è una rete tridimensionale di proteine e altre macromolecole, e sta emergendo come fattore cruciale nella fibromialgia. Essa supporta le cellule, e gioca un ruolo fondamentale nella trasmissione dei segnali dolorosi. Anomalie o alterazioni nella matrice extracellulare potrebbero contribuire alla sensazione di dolore e ai sintomi associati alla fibromialgia.
Queste sono alcune delle principali teorie. La ricerca continua e ogni giorno siamo un passo più vicini a comprendere meglio questa condizione. Il puzzle non è ancora completo, ma si stanno mettendo insieme sempre più pezzi!
Medicina Integrata e Sistemica: La Fibromialgia nell'era moderna
La medicina integrata e sistemica mira a considerare l'individuo nella sua interezza, piuttosto che focalizzarsi solo sulla malattia o sui sintomi specifici.
Questo approccio è particolarmente rilevante per patologie come la fibromialgia
La medicina integrata combina trattamenti convenzionali con terapie complementari che hanno dimostrato di essere sicure ed efficaci. Alcuni esempi ne sono la medicina tradizionale cinese e l’agopuntura.
La medicina sistemica riconosce che il corpo funziona come un sistema integrato e che i disturbi in una parte del sistema possono influenzare altre parti. Questo è particolarmente pertinente per la fibromialgia, data la sua natura complessa. L’obiettivo è ripristinare l'equilibrio tra i vari sistemi del corpo, come l'asse ipotalamo-ipofisi o l'equilibrio tra sostanze ossidanti e antiossidanti, per gestire l’infiammazione e il dolore che contraddistinguono questa invalidante sindrome.
Trattamenti
La fibromialgia è una condizione complessa e, proprio come un puzzle, necessita di diversi pezzi per comporre il quadro completo. Oltre ai trattamenti convenzionali, come antidepressivi e miorilassanti, esistono approcci innovativi come la riprogrammazione posturale, l'integrazione di nutrienti e le terapie “mind-body”.
Queste sono le varie opzioni dell’Approccio Sistemico:
Antidepressivi: Potrebbe sorprenderti scoprire che gli antidepressivi non vengono usati solo per trattare la depressione! In effetti, aiutano a regolare alcuni messaggi chimici nel cervello che influenzano il dolore.
Miorilassanti come la Ciclobenzabina: Questi sono medicinali che rilassano i muscoli. La Ciclobenzabina, ad esempio, aiuta a ridurre gli spasmi muscolari, cioè le dolorose contrazioni involontarie
Infiltrazioni: Alcune terapie più "tecnologiche" possono aiutare. I blocchi anestesiologici, ad esempio, utilizzano anestetici per bloccare temporaneamente il dolore e rimodulare la percezione del dolore stesso

Psicoterapia: A volte, parlare dei propri problemi e sentimenti può fare una grande differenza. Un terapeuta può offrire supporto e strategie per gestire meglio il dolore e le sfide emotive associate alla fibromialgia.
Riprogrammazione posturale: Questa è una sorta di "ginnastica" per il corpo, che aiuta a trovare e mantenere posture che riducono il dolore e lo stress sui muscoli e sulle articolazioni.
Nutrizione e Integrazione di nutrienti: A volte il nostro corpo, oltre ad una dieta equilibrata, ha bisogno di un piccolo aiuto esterno per stare al meglio, e l'aggiunta di Magnesio, Carnitina, PEA e altri nutraceutici può aiutare il corpo a funzionare meglio e ridurre il dolore. La Ademetionina, per esempio, è una sostanza presente naturalmente nel nostro corpo e aiuta a migliorare l'umore e ridurre il dolore
Attività fisica: Mantenersi in movimento è essenziale. Una combinazione di esercizi di riabilitazione per rafforzare i muscoli e attività cardio, come camminare o andare in bicicletta, può fare miracoli per il benessere generale.
Terapie Mind-Body: La meditazione, lo yoga e la terapia cognitivo-comportamentale possono aiutare a gestire lo stress, migliorare la qualità del sonno e affrontare l'ansia o la depressione associata alla fibromialgia
Bagno caldo al mattino: Immagina di immergerti in una vasca d'acqua calda e rilassante. Questo semplice gesto può aiutare a rilassare i muscoli tesi e dare una piacevole sensazione di benessere per iniziare la giornata.
Approccio integrato: L’agopuntura e i suoi vantaggi
L'agopuntura, una pratica millenaria, si sta rivelando un'opzione terapeutica preziosa per molti pazienti con fibromialgia. Può aiutare a ridurre il dolore e a migliorare la qualità della vita, modulando le vie del dolore a livello centrale. Inoltre, l'agopuntura può influenzare il sistema nervoso autonomo, che a sua volta può avere effetti positivi sulla regolazione dell'infiammazione, sul microbiota intestinale e sulla qualità del sonno. A differenza dei farmaci e di altri trattamenti, l'agopuntura non ha effetti collaterali, il che la rende una buona opzione per la maggior parte delle persone.
Cosa ci riserva il futuro?
La fibromialgia, pur essendo una condizione complessa, può essere gestita con una combinazione di trattamenti. L'approccio integrato e sistemico alla fibromialgia riconosce la necessità di un piano di trattamento olistico e personalizzato. Con una comprensione sempre più profonda della fibromialgia, la medicina sta progredendo verso trattamenti più efficaci e personalizzati. L'integrazione di terapie convenzionali e complementari offre una luce di speranza per chi soffre.
Vuoi saperne di più?